Piriformis syndrome might sound complex, but it’s a fairly common cause of hip and buttock pain. This blog aims to explain what piriformis syndrome is, why it happens, and how it’s diagnosed and treated. You’ll get a clear look at the anatomy of the hip and understand why the piriformis muscle and sciatic nerve are often at the centre of this issue. Whether you’re experiencing symptoms or just curious, we’ll guide you through everything from recognising the signs to the best treatment options, including some handy tips you can try yourself.
Anatomy of the hip and muscular structures
The hip joint is formed from by the articulation of the large ball-shaped head of the femur (long bone of the thigh) and the cup-shaped socket of the pelvis (called the acetabulum).
Anatomy of the Piriformis Muscle and the Sciatic Nerve
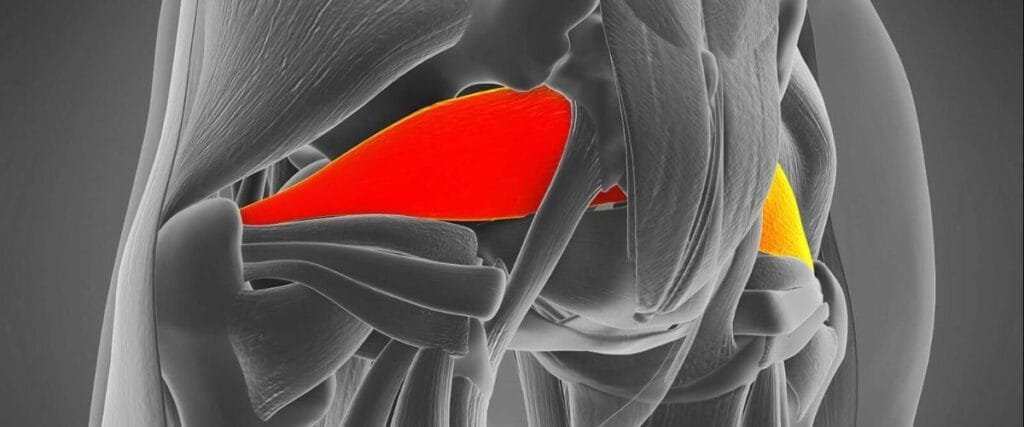
The piriformis muscle is pyramidal in shape and originates from the anterior surface of the S2–S4 sacral (lower vertebra), the capsule of the sacroiliac joint (joint between the sacrum and the pelvis) and the crest of the hip. It then attaches at the greater trochanter of the femur (Khan & Nelson, 2018).
The deep gluteal muscles all contribute to external rotation of the hip. They are covered dorsally by the gluteus maximus and are only seen in cadaveric specimens where this muscle has been dissected away. Piriformis is the most superior muscle of the deep gluteal group.
The main function of the piriformis muscle is abduction and external rotation of the femur, so it effectively assists in bring the leg out to the side and also in turning the out. The piriformis can be a large generator of pain and also be very sensitive due the fact that the sciatic nerve typically passes inferior to the piriformis muscle and then divides to innervate the lower limb.
What is piriformis syndrome?
Piriformis syndrome is a peripheral neuritis of the sciatic nerve caused by an abnormal condition of the piriformis muscle and is characterized by hip and buttock pain. Effectively, piriformis syndrome is a form of ‘sciatica’ caused by compression of the sciatic nerve by the piriformis muscle (Probst et al, 2019).
It was thought that differences in structural anatomy of the sciatic nerve may contribute towards piriformis pain however, a large recent retrospective study found no relationship was identified between sciatic nerve variants and piriformis syndrome (Bartret et al, 2018).
The condition is often mis-diagnosed in the clinical setting and commonly over-diagnosed. Piriformis syndrome can “masquerade” as other potentially more common dysfunctions, such as intervertebral disc issue, lumbar radiculopathy, sacral dysfunctions, sacroiliitis, sciatic disorders, and trochanteric bursitis (Boyajian-O’Neill et al, 2008).
It is estimated that at least 6% of patients who are diagnosed as having low back pain actually have piriformis syndrome however, the range may vary widely between 5- 36% depending on the assessment criteria (Boyajian-O’Neill et al, 2008).
How do I know if you have Piriformis syndrome?
Symptoms can include:
- Pain in sitting
- Pain through the sacrum, gluteal region and thigh
- Pain with single leg movements
- Pain when getting up from sitting or squatting
- Pain in the contralateral (opposite side) of the sacrum
- Numbness in the foot
- Weakness in the leg
- Abdominal, pelvic or inguinal (groin) pain
- Pain with bowel movements
- Low back pain
An updated systematic review (Hopayian & Daniellyan, 2017) reported the commonest features were: buttock pain, pain aggravated on sitting, external tenderness near the greater sciatic notch and pain on any movement increasing piriformis muscle tension, and limitation of lifting up the same side leg in a straight line.
How do we diagnose piriformis syndrome?
Delay in diagnosing piriformis syndrome may lead to pathologic conditions of the sciatic nerve, chronic dysfunction, and compensatory changes resulting in pain, paraesthesia, hyperesthesia, and muscle weakness. The challenge for Physiotherapists is to recognize symptoms and signs that are unique to piriformis syndrome, enabling appropriate treatment in a timely manner.
Clinical examination
A clinical examination is used to inform the physiotherapist of the factors involved in the development of your symptoms. It is used to develop a hypothesis as to why you are experiencing your pain and to provide a treatment plan to address these issues.
A clinical interview is used to understand your situation. You will be asked questions including how and why your pain started, what aggravates and eases your symptoms and how long have you been experiencing pain. A full medical history, including medication history where applicable, will be taken.
A physical examination is then completed and includes lumbar and hip joint range of movement testing, strength and flexibility of the surrounding musculature, palpation (feeling) of different structures of the lumbar spine and hip. A series of functional testing is also completed which often include squatting, single leg balance, gait analysis and running analysis (if you are a runner) and provocation tests for pain arising from the sacroilliac joint. In addition, special neurodynamic tests of the lower limb will be undertaken including a full lower limb neurological screen (reflexes, dermatomes and myotomes).
This process provides a wealth of information about what is causing your symptoms and can lead to a diagnosis of piriformis syndrome. Where symptoms are chronic or where diagnosis is still unclear, specialist imaging is often required to fully confirm the diagnosis and exclude other causes of pathology.
Diagnostic imaging
X-ray
This is commonly used to assess bone and joint structure of the hip and lumbar spine. X-ray is an excellent tool for assessing the shape of the bones of the hip joint, highlighting any structural changes, sinister pathology as well as the quality of the joint space and presence of fractures including stress reactions.
Magnetic resonance imaging (MRI)
MRI imaging is highly accurate at assessing both bone and soft tissue pathologies. MRI imaging can accurately demonstrate and measure both the size of the piriformis, size and variation in the sciatic nerve (Bartret et al, 2018) and any inflammation. An MRI can take between 30 minutes and an hour and involves you lying, motionless in a large cylinder. An MRI takes a series of images of your hip to create a detailed 3D image of your hip architecture
Diagnostic ultrasound imaging
Diagnostic ultrasound imaging is able to visualise the outer edge of the hip joint and visualise inflammation and swelling associated with piriformis syndrome. It also has the added benefit of being able to visualise the hip while moving and is therefore of great benefit when assessing for pain during certain movements.
Diagnostic musculoskeletal ultrasound imaging is it is an excellent imaging tool for assessing for soft tissue hip pathology (Cheatham et al., 2016) as well as being useful for measuring the size and thickness of structures such as the piriformis muscle and the sciatic nerve.
Complete has a highly skilled team of clinicians who have extensive experience of performing diagnostic ultrasound and ultrasound guided injections. During your assessment, your clinician will use both clinical assessment and diagnostic imaging to help diagnose the cause of your hip pain and to locate the piriformis.
If you would like more information or would like to book an appointment please contact us on 0207 482 3875 or email injections@complete-physio.co.uk.
How do we treat piriformis syndrome?
Piriformis syndrome normally responds very well to physiotherapy.
- A personalised, progressive rehabilitation program including mobility and strengthening exercises for the gluteal region and supporting structures.
- Advice on activity modification to minimise the chance of irritating your symptoms.
- Movement re-education – this may include assessment and modification of functional movements and sporting activities.
- Soft tissue release techniques may also be used to reduce pain and increase flexibility around the hip.
- Acupuncture and dry needling techniques can be employed to desensitise the region.
Here are a few top tips you may wish to try yourself:
- Avoid aggravating positions – prolonged periods of sitting and crossing your legs are often associated with irritating the piriformis region by loading and causing pressure on the sciatic nerve. Try to sit evenly and where possible adopt a standing position for periods to work.
- Try to work out what functional movements or exercises cause a flare-up of symptoms. Modify these where possible or stop for a period of time. You can consult your physiotherapist or personal trainer for alternatives.
- Try gently stretching your gluteal muscles, piriformis, calf and hamstrings.
- Pilates-type exercises can also be helpful to engage the core and postural muscles in addition to strengthening your gluteal region.

If physiotherapy treatment has been ineffective at reducing pain and symptoms and the diagnosis has been confirmed on imaging then an ultrasound-guided injection may be appropriate for you.
Patients who respond particularly well to the inclusion of corticosteroid injections normally have pain that:
- wakes you at night and affects your ability to go to sleep
- is limiting your ability to complete daily living tasks including work and leisure activities.
- affects your ability to partake in physiotherapy rehabilitation
Ultrasound-guided corticosteroid injection
Ultrasound-guided corticosteroid injection is an effective evidence-based treatment option for persistent pain associated with piriformis syndrome and has been very well described in literature and studies (Misirlioglu et al, 2015: Smith et al, 2006). Jeong et al (2015) demonstrated that 65% of patients reported significant improvement following an ultrasound guided injection. During an ultrasound-guided injection, a needle is accurately placed into the piriformis. A small volume of corticosteroid (a potent anti-inflammatory medication commonly used in musculoskeletal injection therapy) is combined with a short-acting local anaesthetic. An ultrasound-guided injection should provide significant pain relief for a 6-8 week period and pain reduction for at least 12 months (Masala et al, 2011) after which physiotherapy input should prevent re-occurrence.
Injection therapy should not be used as a stand-alone treatment. An ultrasound-guided injection provides you with a pain-free ‘window of opportunity’ allowing you to rehabilitate you’re the issue effectively. Complete-physio recommend a course of physiotherapy start within two weeks after injection to ensure optimum results.
At Complete, our clinicians are highly experienced, skilled, and leaders in their field. We offer a same-day service for all ultrasound-guided injections, ensuring expert care and precision.
You do not need to be referred by a GP and you do not need to bring a prescription with you. Your treatment includes a full and accurate assessment, diagnostic imaging, medication prescription, ultrasound-guided injection and a comprehensive clinical letter. If you would like more information or would like to book an appointment please contact us on 0207 4823875 or email injections@complete-physio.co.uk.
Other Hip Conditions:
- Iliopsoas Tendinopathy/Bursitis
- Trochanteric Bursitis
- Osteoarthritis of the Hip
- Proximal hamstring tendinopathy
- FAI
References

