If you’re suffering from painful, swollen joints due to conditions like osteoarthritis or rheumatoid arthritis, or have suffered a significant muscle tear or haematoma such as ‘tennis leg’, an aspiration, performed under ultrasound guidance, can provide rapid pain relief and restore mobility.
What Is Ultrasound-Guided Aspiration?
Ultrasound-guided joint aspiration involves using real-time ultrasound imaging to accurately guide a needle into a swollen joint or soft tissue region/haematoma. Removing this excess fluid helps alleviate pain, reduces swelling, and often improves mobility.
Why Choose Ultrasound Guidance for Aspiration?
The traditional method of aspiration relies on palpation (feeling the swelling) and anatomical landmarks to guide the needle, which can lead to less accurate needle placement and poorer outcomes. Ultrasound guidance provides clear visualisation of the target tissue and needle, ensuring precision and improving the effectiveness of the procedure.
Key Benefits of Ultrasound-Guided Aspiration:
- Enhanced accuracy: Ultrasound allows for precise needle placement, ensuring optimal fluid removal.
- Increased safety: By visualising surrounding tissues, we can avoid causing damage to delicate structures like nerves and blood vessels.
- Less pain and discomfort: The procedure is quicker and less traumatic due to the precise needle placement.
- Improved diagnostic value: Ultrasound ensures fluid is aspirated from the correct area, aiding in diagnosing the source of the pain.
- Better outcomes: Research shows ultrasound-guided aspirations can be up to 300% more effective than unguided techniques, with faster symptom relief.
Conditions That May Require Aspiration
Here are some common conditions where joint aspiration is beneficial:
- Osteoarthritis: A degenerative joint condition where cartilage breaks down, leading to pain and inflammation. The knee is the most common joint that we aspirate at Complete.
- Rheumatoid arthritis: An autoimmune disease that causes chronic inflammation of the joints.
- Gout: A form of arthritis caused by the accumulation of uric acid crystals in the joints.
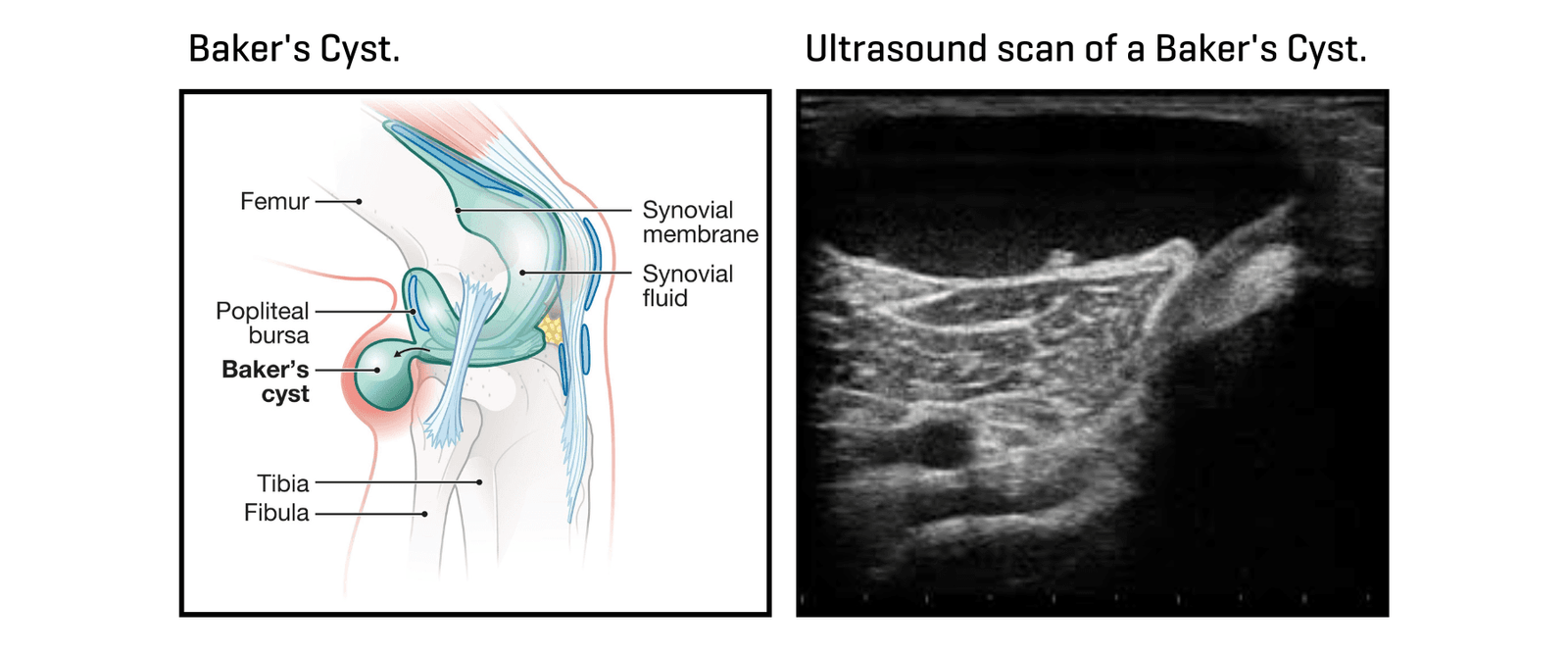
- Baker’s cyst: A fluid-filled swelling at the back of the knee, often associated with arthritis or meniscal tears. Aspirating the cyst can relieve pressure and discomfort.
- Muscle tears (haematoma): In cases of large collections of blood (haematomas) forming after muscle tears, such as in the calf (tennis leg), quadriceps, or hamstrings, aspiration can provide pain relief and improve the quality and speed of healing.
Can I have a steroid injection at the same time as an aspiration?
Yes, you can have a steroid injection at the same time as a joint aspiration, but this is generally recommended only for joints rather than soft tissue aspirations. Joint fluid often contributes to joint pain, especially when inflamed. Combining aspiration with a steroid injection in a joint can help relieve pain, reduce inflammation, and may improve outcomes by lowering the chance of fluid returning. However, for soft tissue aspirations, it’s typically not advised to add a steroid injection due to differences in tissue response and the risk of complications.
Real-World Success Story: A Triathlete’s Journey
One of our patients, a competitive triathlete, was struggling with pain and swelling at the back of the knee, which was making cycling nearly impossible. After an ultrasound scan, we diagnosed a Baker’s cyst and immediately performed an aspiration, draining the fluid during our one-stop clinic—from assessment to treatment in a single session.
“I was in so much pain with a swollen knee and couldn’t train or even ride my bike without discomfort. When I came to Complete Physio, they diagnosed a Baker’s cyst on the spot and did the aspiration right then and there. The relief was immediate—I was over the moon! The whole process was fast, efficient, and pain-free, and I was back to competing in no time. Amazing service!” – Marcus S, 34, London
When Should Joint Aspiration Be Avoided?
There are some situations where joint aspiration should be avoided:
- After a joint replacement: We are unable to aspirate the knee once a replacement has been performed.
- Recent surgery: If you have had knee surgery and are still under the care of an orthopaedic specialist, we cannot perform an aspiration unless the case has been discussed with your surgeon.
- Uncertain diagnosis: If there’s uncertainty about the cause of the swelling, or if a significant injury such as a fracture is suspected, further imaging may be required before proceeding with aspiration.
If further imaging is needed, such as an MRI, we can refer you directly—there’s no need to go through your GP. MRI scans cost around £300. Before recommending further imaging, we will always perform a diagnostic ultrasound scan, but if we need more detailed information, an MRI is the next step.
What is Aspirated?
The fluid we aspirate from a joint is typically synovial fluid, a thick liquid that lubricates the joints and reduces friction. In an inflamed joint, this fluid builds up and causes pain. We examine the fluid’s colour, viscosity (thickness), and composition to check for any concerning features. For example, blood mixed with synovial fluid may indicate trauma, while signs of infection are rare but possible. The amount of fluid removed can vary significantly, from 5mL to 150mL, but typically around 10-30mL is aspirated. In one instance, we aspirated 140mL from a patient’s knee, resulting in immediate relief.
Once we have aspirated the joint, we may consider injecting a steroid to help reduce inflammation and prevent recurrence of the fluid/swelling. If you have osteoarthritis, we might recommend a hyaluronic acid injection to improve joint lubrication, or in some cases, we combine steroid and hyaluronic acid. The choice of treatment depends on the assessment findings and what we are trying to achieve in managing your condition.
If we aspirate a haematoma following a muscle tear, it is normally serous blood stained fluid from when the bleeding occurred.
What to Expect During the Procedure
- Assessment: A thorough examination and diagnostic ultrasound scan will be performed to identify the source of the swelling.
- Preparation: The area will be cleaned, and you will be positioned comfortably for the procedure.
- Needle insertion: Guided by real-time ultrasound, we will insert a fine needle and drain the excess fluid. Local anaesthetic can be used when necessary to reduce any pain associated with the procedure.
- Post-procedure care: You may be advised to rest the joint for a short period after the aspiration, and in some cases, follow-up physiotherapy may be recommended to help prevent the fluid from returning. We may ask you to compress the region with a bandage for a few days to prevent the fluid from returning.
Joint Aspirations – Frequently asked questions (FAQ’s):
Do I need a referral from my GP for joint aspiration?
No, we can assess and treat you without the need for a GP referral.
Do I need an MRI or X-ray beforehand?
Not always. We usually diagnose the issue with an ultrasound scan. If necessary, we can refer you directly for further imaging, such as an MRI, which costs approximately £300.
What are the benefits of joint aspiration?
Joint aspiration can provide rapid pain relief by removing the excess fluid that causes irritation and inflammation. It can also aid in diagnosis based on the fluid’s appearance and characteristics.
What are the risks of joint aspiration?
Although rare, the risks include:
- Infection: this is extremely uncommon, and we take all necessary precautions to avoid an infection
- Bleeding: Minor bleeding may occur, especially if you’re on blood-thinning medication, so it’s important to ensure your medication is well-managed.
- Pain: Some discomfort is expected during and after the procedure, but we minimise this through the use of local anaesthetic and precise technique.
Do I need more than one aspiration?
Most patients only need one aspiration. However, in cases like severe osteoarthritis, multiple aspirations may be required. Combining the aspiration with a steroid injection can reduce the need for repeat procedures.
Conclusion
Ultrasound-guided aspiration is a safe, accurate, and effective procedure for relieving pain and swelling caused by conditions such as osteoarthritis, rheumatoid arthritis, gout, muscle tears and Baker’s cysts. By removing the irritating fluid, you can experience immediate pain relief and improved function.
For more information or to book an appointment, contact Complete on 020 7482 3875 or email info@complete-physio.co.uk.


