what is iliotibial band (ITB) friction syndrome
Iliotibial band (ITB) friction syndrome is a very common running injury, hence it is often referred to as “Runner’s Knee”. It can be a stubborn, tricky injury to fully resolve and is a common reason people struggle to get their longer training runs completed particularly in the last 4-6 weeks of their marathon training. It is also a common reason why people start but do not finish the marathon.
Approximately 20% of people that enter a marathon get injured and do not reach the starting line. ITB friction syndrome or “Runner’s knee” is one of the most common injuries that we see in the run up to the marathon.
Symptoms of ITB Friction Syndrome?
ITB friction syndrome is often described as a condition where the ITB ‘rubs’ over the lateral femoral epicondyle (a boney prominence on the outside of the knee), which causes pain and inflammation in that region.
This is a very simplistic view of the issue and there are many factors that also need to be assessed and more importantly considered to successfully treat ITB friction syndrome.
How to treat ITB Friction Syndrome? What is ITB friction syndrome?
At Complete Physio, every year we see a lot of ITB friction syndromes during the training phase for the marathon and the majority resolve with physiotherapy alone.
Physiotherapy is likely to involve:
- ITB Friction syndrome focused exercises for both the hip and knee (and potentially ankle/foot)
- Stretching exercises for key lower limb muscles
- Modification of training loads
- Running analysis and footwear assessment
- Hands on treatment to optimise soft tissue mechanics and balance
- itb friction syndrome taping and/or advice regards insoles (orthotics)
If you have exhausted physiotherapy or you quite simply are running out of time before the event, then read on!
How we diagnose ITB Friction Syndrome
Before we discuss the other treatment options available, we must first look specifically at diagnosis. At Complete we believe getting the right diagnosis is the most important part of the process. Without the right diagnosis, you will not implement the right treatment. If you are not improving, we must firstly consider if you do actually have “ITB friction syndrome”.
There are many conditions that can mimic the pain of ITB friction syndrome. These include:
- Patellofemoral knee joint pain
- Patella tendinopathy
- Lateral knee joint pathology such as a lateral meniscus tear
- Stress fracture of the distal femur
- Popliteal tendinopathy
- Osteoarthritis
- Plica

At Complete, our team of clinical specialist physiotherapists will carry out a full clinical assessment, and also a diagnostic ultrasound scan (at no extra charge). Please ensure at the time of booking you inform the bookings team that you need an ultrasound scan, Diagnostic ultrasound is excellent at looking under the skin and identifying exactly which structures are involved in driving your pain. This will help us to confirm the diagnosis and provide a targeted approach to your treatment.
If we feel you do have pain arising from the ITB and/or surrounding structures, we will look specifically at three things when we carry out the diagnostic ultrasound scan (this can be a bit technical!).
- The first is to look for thickening of the ITB itself. This can be measured and compared to the other side on ultrasound. This normally happens in more chronic (when you have had the problem for several months) presentations.
- The second thing we will look for is fluid underneath the ITB, between the ITB and the lateral femoral condyle (the bony bit on the outside of the knee). If there is fluid this is known as a bursitis. This bursa gets inflamed as your training ramps up and can be difficult to settle down with physiotherapy alone.
- One of the main things that we see in clinic, when the pain associated with an ITB friction syndrome is not improving, is fluid tracking up from the knee joint itself. The diagnostic ultrasound scan is able to assess for joint fluid tracking up from the outside of the joint and sitting between the ITB and the femoral condyle (bone on the outside of the knee). This is demonstrated on the image below. This is essentially a pseudo-ITB friction syndrome, i.e., not a true ITB friction syndrome and so is unlikely to improve with the typical treatment approaches for ITB friction syndrome. This causes pain on the outside of the knee (mimicking ITB issues) but is actually secondary to an overload of the outside of the knee joint itself. This is why getting a correct diagnosis is so important!
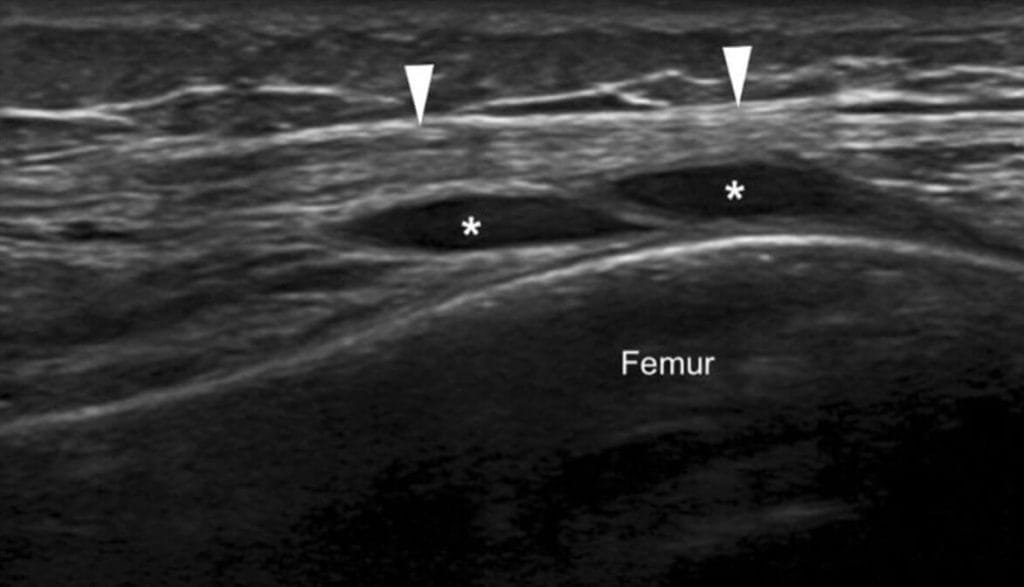
Longitudinal Ultrasound Image of the ITB with joint fluid underneath (*) tracking from the lateral (outside) of the knee joint
What other treatment options are available for you?
If you are experiencing ongoing pain, we would advise you to book in with one of our clinical specialists who are also trained in diagnostic ultrasound. Inform our bookings team that you require a scan at your appointment. On your first appointment we will carry out a clinical assessment and a diagnostic ultrasound scan.
This will reveal exactly what is happening and why you are getting pain. From the scan we will answer the three key questions listed above. At this point, once we know exactly what is going on, a decision on an ultrasound guided steroid injection can be made.
What if we are unsure about the diagnosis?
If we are still unsure, then we can carry out an ultrasound guided local anesthetic injection. This is where we place a very small amount of local anesthetic between the ITB and the condyle, under ultrasound guidance, and ask you to run (this is perfectly safe).
If your pain does go when you run, then the symptoms are likely to be coming from the source that we injected. This is very useful diagnostically and would indicate that a guided steroid injection may be appropriate. Read on.
An ultrasound guided steroid injection should be considered if:
- Your pain is not improving despite activity modification
- You have not improved with a course of physiotherapy
- You have had a scan to confirm the exact diagnosis
- You are running out of time and do not have time to engage in a course of physiotherapy prior to the marathon
The pros and cons of an ultrasound guided injection will be discussed with you during your appointment. At Complete, although we do want to get you through the race, we will not do anything that compromises the long-term health of your knee.
What is an ultrasound guided steroid injection and how does it help the pain from ITB friction syndrome?
Steroid injections are strong anti-inflammatories, targeted directly to the area of concern. This will reduce the inflammation between the ITB and the femoral condyle and works particularly well if there is a bursitis or thickening of the ITB (seen on ultrasound). If the pain is coming from the joint, then the joint will be injected, rather than the ITB. An injection can provide rapid pain relief and get you back to running. We normally advise anything between 3-7 days off running after the injection depending on the scan findings and how severe your problem is.
An ultrasound guided injection uses an ultrasound machine to guide the steroid to the target tissue. The target tissue is often a few millimeters in size and therefore guidance is essential to get the desired outcome. From our experience ultrasound guided injections have improved outcomes compared with ‘blind’ injections (this is where the needle is not guided during the procedure). Steroid injections can help to relieve the pain, but in addition your clinician will guide your return to running to ensure you do not overdo it.
Prolonged ITB Friction Syndrome Pain?
On the morning of the marathon, if you are still suffering, Complete Physio run a specific injection clinic. In this clinic, prior to the race, we carry out a long-lasting local anaesthetic injection under ultrasound guidance between the ITB and the femoral condyle (the bone on the side of the knee) into the bursa, to ensure that you do not get pain during the marathon. This can only be done once for the day itself and not the training runs. The pros and cons of doing this on the day will be discussed with you at the time.
The pros and cons of doing this on the day will be discussed with you at the time. If you would like to discuss this in more detail, please email info@complete-physio.co.uk
If you have any questions, and/or you are struggling with ITB friction syndrome, please do not hesitate to contact info@complete-physio.co.uk
There are conditions that can mimic the pain of ITB friction syndrome. For more information about these conditions click the links below:
- Patellofemoral knee joint pain
- Patella tendinopathy
- Lateral knee joint pathology such as a lateral meniscus tear
- Osteoarthritis
Chris Myers, Clinical Director at Complete Physio and ex-British Athletics physiotherapist, discusses ITB friction syndrome. Chris outlines what it is, how it is diagnosed (this is very important) and what you can do it about, in particular with one month to go before the marathon, and even on the day of the event itself!